This essay appears in print in The Politics of Care.
If there is one thing this pandemic is making abundantly clear it is that our individual health is interconnected—to each other, to our political and economic systems, to the broader ecology, and the other species we share the planet with.
The pandemic, after all, has made disturbingly visible that we are all only as healthy as our societal support systems. As the writer Anand Giridharadas put it: “Your health is as safe as that of the worst-insured, worst-cared-for person in your society.” In the United States, decades of cuts to our nation’s social safety net have left us struggling to respond to COVID-19 with an appallingly inadequate public health sector, almost nonexistent job security, and a government more concerned with maintaining profits than saving people’s lives.
At the same time the pandemic reveals that our bodies function more like sponges than fortresses. In a variety of visualizations, we see our bodies extending beyond their usual bounds: graphics of our coughs, sneezes, and even breath show how far beyond our own skin our bodies reach; the six-foot rule of social distancing a daily acknowledgement that our bodies not only leak and ooze, but that they absorb the conditions of others. Our sensitivity to each other’s physical presence has never felt more visceral.
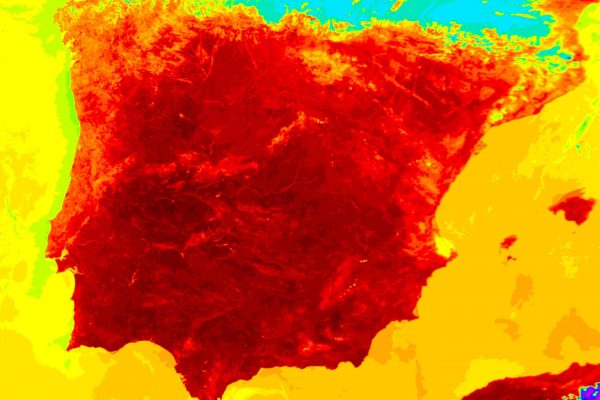
And the pandemic exposes connections beyond our species. We know that environmental destruction aided the conditions that led to this outbreak: deforestation, rising temperatures, and the loss of habitat, all forced species into closer contact with each other, including with our own. It is increasingly clear that this virus, just like the many other zoonotic viruses that have come before, jumped from one species to another (in this case, to humans, likely from bats or pangolins), aided by the consumption of wild animals and the global increase in unsanitary and brutal factory farms.
The spread of the virus reminds us that our bodies are enmeshed with the bodies of other creatures and ecosystems.
The spread of the virus from humans to cats, dogs, and even tigers at the Bronx Zoo has brought us crashing back into the animal world, reminding us that our bodies are enmeshed with the bodies of other creatures and ecosystems. To this point Giridharadas might have added, your health is as safe as the most endangered species, the most exploited industrialized food animal. Or, that of the most clear-cut forest, the worst-regulated and polluted ecosystem.
When Public Health And Environmental Protection Were One
The idea that our health is connected to and interdependent with the health of other people, environments, and social structures is of course not new. Indeed, a brief look at the shared roots of public health and environmental protection exposes shows that such connections helped shape the mandates of government agencies for over a century.
While it could be argued that the origins of both the public health and environmental movements date as far back as the earliest drainage systems, toilets, and water systems in ancient history, the sanitary movement and the social reformers of the nineteenth century deserve an abundance of credit for birthing environmental concern in this country. These reformers recognized the role of dirty water, smog filled air, piling waste, and inadequate housing as serious threats to human health and well-being—particularly among the urban poor.
The first U.S. boards of health were established after epidemics of cholera and yellow fever broke out in the late eighteenth century. Such diseases were claiming thousands of lives, with outbreaks often occurring in areas with dirty water and unsanitary conditions. As with the coronavirus pandemic, people most vulnerable to infectious disease already endured poverty, environmental contamination, structural racism, and inadequate health care as pre-existing conditions. Throughout the nineteenth century the poor were largely blamed for diseases that decimated their communities, but social reformers identified poverty, overcrowding, unhygienic housing, and inadequate waste disposal as the cause; they advocated for the construction of safe water supplies, sewage systems, and street cleaning. Early boards of health became models for local and state public health agencies, which among other things became responsible for controlling disease through sanitation, air pollution control, and clean water supplies.
In the nineteenth century, environmental health, public health, and occupational health were largely understood as a single discipline of health seurlty.
At this time environmental health, public health, and occupational health were largely understood as a single discipline, which emphasized disease prevention and social reform and which focused on the living and working conditions of people in urban communities. By the beginning of the twentieth century, however, the field began to separate into the three distinct arenas we know today, all of which were increasingly informed by advances in science and technology. Still, these disciplines were connected enough that by the 1930s labor movements advocating for what historian Jennifer Klein identifies as “health security” in the New Deal era would often include dimensions of all three. Tracing the history of the labor movements early struggles for a more expansive welfare state, Klein, writes in her book For All These Rights (2003) that “the politics of the New Deal put security at the center of American political and economic life.” “Labor,” she explains, “saw health security as part of a broad economic security project” with policy proposals that included “occupational safety, industrial health, and public health demands.”
Klein details how labor’s multifaceted visions of health security were thwarted by the emergence of such incentives as employee benefits programs, including employer-based health insurance, a much more limited effort. U.S. industry aggressively fought to reduce the links between workers and the state, by offering benefits tied to employment. After World War II, Klein writes, “American business firms and commercial insurance companies became partners in creating and expanding nonstate alternatives to public social insurance.” As well as detailing the history that has left workers in the United States at the mercy of this employment dependent system, Klein’s project also exposes that there once was a far broader vision of what health care could look like, and it included environmental public health.
“The health security movement’s emphasis on community-based models could have changed the American conception of health care in significant ways,” Klein writes. “Less focused on technology intensive hospital care, they might have allocated resources and attention more equally between clinical medical services and policies addressing the economic and environmental factors that affect health.” As the coronavirus lays bare not only the inadequacies of employee-based health insurance and the U.S. social safety net but the economic and environmental impacts on health as well, the urgency of reclaiming this more expansive vision of health security is undeniable.
Breaking Apart
While environmental protection drifted away from its roots in public health and social reform, and as organized labor’s expansive visions for health care faded, the economic growth of post-war America would increasingly take a terrible environmental toll. As the effects of industrial pollution became visible in smog-filled skies, contaminated rivers, and shrinking wild spaces, a growing percentage of the public became concerned with environmental protection, sparking the environmental movement of the 1960s and 1970s.
Yet, despite the clear public health implications of the growing environmental crises, the burgeoning environmental groups of the time traced their origins not to the health reformers and “sanitary science” champions of the industrial era, many of whom were women, but to the conservation movement of the nineteenth century—a movement, as a myriad of environmental historians have pointed out, shaped by eugenicist, masculinist, and white supremacist ideas. Centering this genealogy had the unfortunate effect of shaping a U.S. environmental movement that for decades focused more on protecting pristine wilderness largely for white leisure, than protecting polluted urban environments and the communities of color living with them.
For decades the U.S. environmental movement focused more on protecting pristine wilderness largely for white leisure, than protecting polluted urban environments and the communities of color living with them.
Responding to pressure from the movement, Nixon created the Environmental Protection Agency (EPA) in 1970, severing public health authority from environmental protection at the policy level. Federal and state level health departments had historically housed responsibility for many of the nation’s environmental programs, including the protection of water and air. Those same agencies dealt with preventive health services, maternal and child health, nursing, health records, statistics, and local health administration. The Nixon administration removed environmental responsibility from these departments, consolidating them into a new agency, in order to put forward a more efficient and comprehensive environmental program.
The creation of the EPA was largely met with excitement; health departments, after all, had often failed miserably to protect the environment, a challenging task given the dearth of environmental regulations at the time. The new structure brought much needed funding and attention to environmental issues. Yet the separation of environmental agencies from public health also led to a steady decline in the role of public health perspectives within them. While a fundamental mission of the EPA to this day is to protect public health, such approaches and leadership have largely been neglected. The Institute of Medicine’s 1988 report, The Future of Public Health, lamented that “The removal of public health authority from environmental agencies has led to fragmented responsibility, lack of coordination, and inadequate attention to the public health dimensions of environmental issues.”
The split arguably helped further separate understandings of the interdependence of human and nonhuman health only a few years before environmental justice and environmental health movements began to advocate for precisely such an understanding. In the late 1970s people whose communities had experienced the severe health impacts from toxic water and air pollution began identifying and challenging the ways environmental harm is distributed along racial and class lines. Ever since then, these movements have asserted that health and racial justice are at the heart of environmental protection, and that the health of people and environments are entangled.
The split between environmental protection and public health has also institutionalized the idea that human bodies and communities are separate from “nature”—that people are impermeable, independent, self-sustaining, and individually bounded entities that can be protected with the right health insurance package. This narrow technocratic structure diminishes understandings of how health and vulnerability to injury are things that cross both species and environmental boundaries and are fundamentally entangled.
The Future Is Disabled
The pandemic is making these entanglements visible, exposing not only our connections—to each other, to other species, to our environments—but also the vectors of connection through bodily vulnerability to illness, dependency, injury, and disability. In previous work I have called this network of connections “disabled ecologies,” the trails of disability that are created, spatially, temporally, and across species boundaries, when ecosystems are contaminated, depleted, and profoundly altered. While disabled ecologies are all around us, emerging from the climate crisis, from long contaminated Superfund sites, from deforestation and fossil fuel extraction, the pandemic’s disabled ecology is forcing a response from a global system that has thus far failed to act on environmental catastrophe.
The pandemic is making these entanglements visible, exposing our connections to each other, to other species, to our environments.
Yet, the response to this pandemic in the United States has often denied our connections and interdependence. From the beginning we have been told with relief that the virus is mostly dangerous for the elderly and those with pre-existing conditions—as if these people are not already us and the ones we love. The conditions that make someone more vulnerable to COVID-19 are of course intimately tied up with poverty, environmental racism, and inadequate health care. Thus while such a sentiment is unabashedly ableist—should we mourn the lives of the healthy and robust more than the lives of the ill and disabled?—it is also deeply racialized, a message to America’s white middle class that they have no need to panic. In addition, we have been alerted to the real possibility that overburdened hospitals with limited medical supplies might withhold treatment from disabled patients with COVID-19. Already disability rights organizations have filed various lawsuits against such rationing guidelines in several states.
The truth is that over 60 percent of the population in the United States has a chronic health condition, and 40 percent has more than one. A disproportionate number of disabled individuals are poor and working-class people of color, employed as “essential workers,” a euphemism that covers up the devastating reality that the majority have no safety net, no health insurance, and no PPE. Essential, and yet dying in vast numbers. Calls for the country to reopen, and for vulnerable people to continue to isolate, only serve to center visions of able, healthy, and independent individuals in a pristine world as the norm, even as the climate crisis and rising global inequity, make an increasing majority of us—and the ecosystems we live with—sick and impaired. The human and nonhuman beings who are ill and disabled continue to be represented as elsewhere. But they are not marginal. They are us.
Meanwhile, the current administration has given a green light to polluters, lifting emissions regulations long set by federal environmental laws. It has offered bailouts to fossil fuel and meat industries, the very industries most responsible for the environmental crises we are facing.
While various news stories have pointed to the decrease in air pollution during the pandemic, evidence suggests that communities living in areas with high industrial pollution are more likely to have higher rates of COVID-19 cases, and that because emissions regulations are not currently being enforced, industries may now be more emboldened than ever to pour ever more toxins into these same areas. The predominantly black communities of Louisiana’s “Cancer Ally,” for example, have some of the highest death rates of COVID-19 in the country. As a recent piece in Vice put it, “The risk factor list for severe coronavirus cases issued by the CDC is a litany of conditions aggravated or caused by pollution: asthma, chronic obstructive pulmonary disease (COPD), heart disease, hypertension, and diabetes.” For communities long on the frontlines of environmental racism, ecological and human harm rise together.
In January 2016, following the popularity of the new slogan, “The Future Is Female,” Alice Wong’s website, the Disability Visibility Project, announced the creation of the hashtag #thefutureisdisabled. On the day the hashtag was announced, Wong wrote “You might wonder, ‘What the hell is The Future Is Disabled?’ Does it sound ominous? Hopeful? Inevitable? What does it mean?” While the trending hashtag was meant as a way of challenging eugenicist legacies—a way of claiming the future for disabled people and disabled perspectives (indeed another variation of the appropriated slogan was #thefutureisaccessible), I always thought of the slogan through an ecological frame—as a way of conceptualizing climate breakdown, mass extinction, and mutation. Since coronavirus has hit the world, it seems to me that the future has arrived far sooner than expected.
Universal Health Care for People and the Planet
For decades disabled communities have taught us that while injury and sickness are fundamental to life, our response to injury and sickness is a societal issue. At this moment—as the vulnerability and dependency of our bodies is so undeniably entangled with the health of ecosystems and other species—it is time to recognize ourselves as an increasingly disabled people in increasingly disabled landscapes. How then should we respond to injury?
We need to rethink the separation of human health from the health of our environments and social welfare systems.
Perhaps, to start, we can rethink the separation of human health from the health of our environments and social welfare systems. What has been lost in breaking off environmental protection from public health agencies and in narrowing an expansive vision of health security to a fight for access to health care?
Imagining a radical expansion of and marriage between environmental remediation and health security likely seems naive under any circumstances, given the U.S’s deeply engrained for-profit health care system and the dismal funding history of the EPA. But today’s extraordinary crises—rising global authoritarianism, spectacular levels of inequality, increasing deregularization, environmental devastation, and a global pandemic—have increased calls for a just response. And activists have already modelled such a vision. Movements for environmental justice, climate justice, indigenous sovereignty, disability justice, as well as new public health frames such as the growing concept of “One Health,” and recent calls for a New Deal for Public Health, are centering the idea that the health of humans is inseparable from the health of the environment. Indeed, a myriad of scientists, medical professionals, activists, and government agencies are telling us that we are facing a global health crisis because the very health of our environments is in extreme peril. The coronavirus pandemic makes clear that struggles for Medicare for All and a Green New Deal are two sides of the same coin. We urgently need them both—and more.
But we also need to rethink our relationship to disability and illness as a society. The future is disabled, but that need not be foreboding. It could signal a future that recognizes and supports our mutual vulnerability as creatures on this planet, a future that is structured around our interdependence with each other and the environments and species we live with, and a future that pursues access for people at all stages of life and abilities. Even if we could miraculously stop the spread of coronavirus and the climate crisis tomorrow, we will be treating the injury to our altered ecosystems and the beings who live with them for years to come. The future is indeed disabled, but what we do in the present will define whether that future can be hopeful.
Boston Review is nonprofit and relies on reader funding. To support work like this, please donate here.