Mind Fixers: Psychiatry’s Troubled Search for the Biology of Mental Illness
Anne Harrington
W. W. Norton, $17.95 (paper)
Desperate Remedies: Psychiatry’s Turbulent Quest to Cure Mental Illness
Andrew Scull
Harvard University Press, $35 (cloth)
In 1990 President George Bush announced that “a new era of discovery” was “dawning in brain research.” Over the next several decades the U.S. government poured billions of dollars into science that promised to revolutionize our understanding of psychiatric disorders, from depression and bipolar disorder to schizophrenia. Scientists imagined that mental illnesses in the future might be diagnosed with genetic tests, a simple blood draw, or perhaps a scan of your brain. New pharmaceuticals would target specific neurochemical imbalances, resulting in more effective treatments. The 1990s, Bush declared, would be remembered as “The Decade of the Brain.”
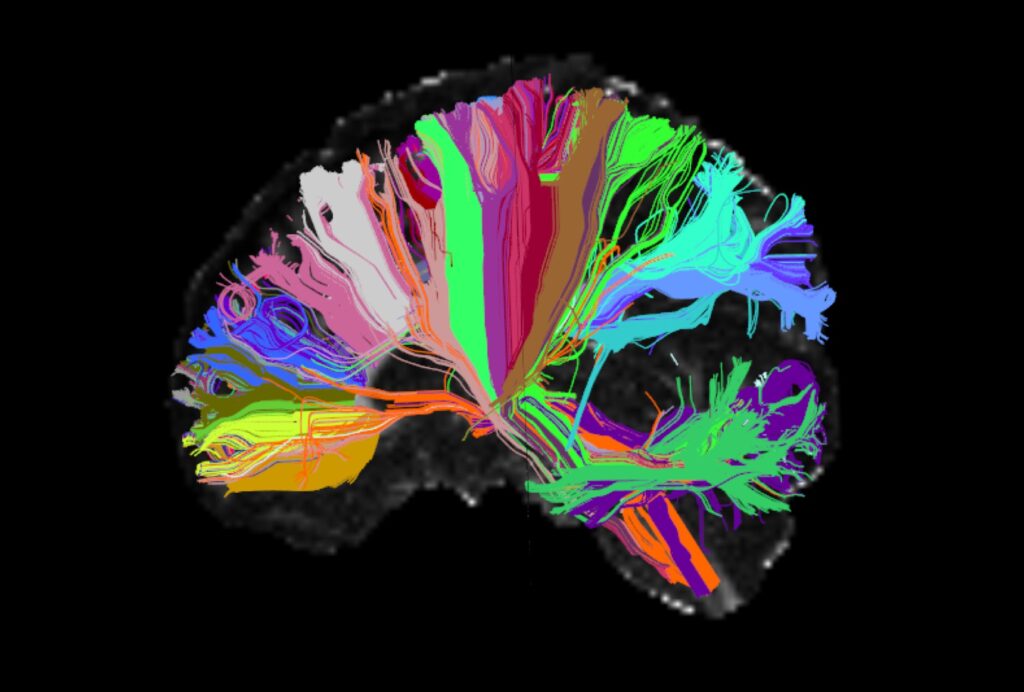
This brave new world of brain research also promised to free us of the stigma and discrimination attached to mental illness and addiction for centuries. Localizing psychiatric disorders in the brain would make them chronic medical diseases—like diabetes and high cholesterol—instead of individual moral failings or deficiencies in character. While it was impossible to predict exactly what the future would bring, there was an overwhelming sense that psychiatric science was going to crack the “mystery” and “wonder” of this “incredible organ,” as Bush called it.
Looking back as a psychiatrist and historian today, I find that these hopes feel quaint. They remind me of other misplaced visions of technological futures from the twentieth century: flying cars, pills for a whole day’s nutrition. The reality of psychiatric practice is far less glamorous than the visions of its future that I grew up with. Thirty years later we still have no biological tests for psychiatric disorders, and none is in the pipeline. Instead our diagnoses are based on criteria in a book, the Diagnostic and Statistical Manual of Mental Disorders (often called, derisively, the “bible” of American psychiatry). It has gone through five editions in the last 70 years, and while the latest edition is almost 100 pages longer than the last, there is no evidence that it is any better than the version it replaced. None of the diagnoses is defined in terms of the brain.
We also have not had any significant breakthroughs in treatment. For decades the pharmaceutical industry has churned out dozens of antidepressants and antipsychotics, but there is no evidence that they are more effective than the drugs that emerged between 1950 and 1990. People with serious mental illness today are more likely to be homeless or die prematurely than at any point in the last 150 years, with lifespans that are 10 to 20 years less than the general population. Biological research has also failed to reveal why psychiatric drugs help some patients but not others. When a patient asks me how an antidepressant works, I have to shrug my shoulders. “We just don’t know, but we do have evidence that there’s about a 30 percent chance that it will help your mood.” Perplexed, one patient responded, “Doesn’t it have to do with neurotransmitters or something?” I sighed, “Yes, that was the theory for a while, but it didn’t pan out.”
And how about stigma? As anthropologist Helena Hansen has argued, the neuroscience of addiction has often reinforced stigma by reducing substance use to an individual problem, instead of the result of structural factors rooted in longer histories of racial violence. American psychiatrists also diagnose Black and Brown patients with disproportionate rates of schizophrenia compared to white patients—a disparity that psychiatrist-sociologist Jonathan Metzl traces to psychiatrists in the 1970s who pathologized Black activism as “psychosis.” Finally, Black patients experiencing mental health crises, including children, are more likely to experience the violence of being physically restrained, tied to their beds in ways that resemble the experiences of asylum patients over a century ago.
In 2015 the former director of the National Institute of Mental Health (NIMH), Thomas Insel, crystallized this disillusionment:
I spent 13 years at [NIMH] pushing on the neuroscience and genetics of mental disorders, and when I look back . . . I realize that while . . . I succeeded at getting lots of really cool papers published by cool scientists at fairly large costs—I think $20 billion—I don’t think we moved the needle in reducing suicide, reducing hospitalizations, improving recovery for the tens of millions of people who have mental illness.
It does not help that academic psychiatry today feels out of touch. Many people have underscored the profound importance of mental health amid the social isolation of the pandemic, racial violence in our society, and the increasingly hyper-competitive culture of schools, sports, and the market. But academic psychiatry’s almost singular focus on brain-based research has meant that the profession has been largely absent from these conversations. And for what? All the “cool papers” on neurobiology have won academic grants and helped professors get promoted, but they have not meaningfully impacted the diagnosis and care of the millions of people suffering psychic distress.
How did we end up here? If we have failed to understand psychiatric disorders biologically, what happens when we examine them historically? Two recent books by historians explore the crisis in biological psychiatry, tracing the political, economic, social, and professional factors that led psychiatrists to attempt to pin the reality of mental illness—and the legitimacy of the profession—on the brain. Written by leading historians in the field, these are big books, in heft and scope, that cover two hundred years of the profession’s failures. They reveal that U.S. psychiatry, across its history, has been dangerously susceptible to hype and “cool,” ranging from enthusiasm for brain dissection in the 1890s to the fanfare surrounding neurotransmitters and genetics a century later.
Understanding the undulating history of psychiatric hype and crisis is crucial today as the profession builds toward its next trend: psychedelics, already heralded as a “renaissance” and psychiatry’s “next frontier.” These two histories demonstrate that the academic and corporate pursuit of such hype has neglected the perspectives of communities most affected by psychiatric research and care, resulting in significant psychological and bodily harm. The strengths and limitations of these important books push academic psychiatrists to reexamine our priorities. They challenge us to envision a future world where the billions of dollars invested in biological research are instead redistributed to the communities who need it most—in order to provide the resources necessary for radically reimagined forms of care that center whole humans instead of just brains.
In Mind Fixers: Psychiatry’s Troubled Search for the Biology of Mental Illness, Anne Harrington argues that the current crisis is just the latest in a long line of failures to discover the biology of mental illness over the last two centuries. In this sweeping study, the history of psychiatry undulates like the boom and bust of a speculative market. First a wave builds with enthusiastic promises of revolutionary breakthroughs that will change psychiatry as we know it. Then the wave collapses, as psychiatrists fail to deliver on those bold promises. Crisis ensues, and after the requisite finger-pointing, the next wave of psychiatric revolution begins to build. Rinse and repeat.
The first “revolution” in American psychiatry that Harrington tracks arrived in the nineteenth century. At the time, large lunatic asylums dominated the psychiatric landscape, such as the Blackwell’s Island hospital on what today is called Roosevelt Island in New York City. These institutions were designed to cure patients with mental disorders by placing them in the hospitable environment of the asylum architectural space. However, a series of journalistic exposés revealed that these asylums were overcrowded and underfunded with patients living in deplorable, instead of therapeutic, conditions. For example, in 1887, journalist Elizabeth Seaman, who wrote under the pen name Nellie Bly, went undercover as a patient in Blackwell’s Island Hospital and exposed horrible acts of brutality in her best-seller Ten Days in a Mad-House. Asylum psychiatry faced a crisis of public trust.
As Harrington explains, European neuroanatomists came to the rescue. Unlike asylum physicians, anatomists were pessimistic about the potential for a cure. Building on eugenic theories, they believed that asylum patients were “degenerates” who were biologically unfit to cope with the stresses of modern life. But they also believed that the mentally ill could provide a service to society after their deaths by offering their brains to science. The dissection of their pathological brains, the anatomists hoped, could reveal the biological causes of mental suffering.
As the asylum transformed from a therapeutic institution into a site for research over the course of the late nineteenth century, thousands of dissections were performed on the bodies and brains of mostly poor patients without their consent. Harrington concludes that they revealed “more or less nothing.” The problem was that neuroanatomists had no idea what they were looking for. The psychiatrist Karl Jaspers summed up these anatomical efforts as a “brain mythology.” Neuroanatomical dissection was a bust.
Abandoning the therapeutic nihilism of neuroanatomists, the second push for biological psychiatry swung to the other extreme. The early twentieth century in the United States was a period of unbridled, desperate experimentation on patients’ bodies in the desperate search for a cure. Andrew Scull’s new book Desperate Remedies: Psychiatry’s Turbulent Quest to Cure Mental Illness gives a chilling account of a period characterized by an “orgy of experimentation.” While covering much of the same historical ground as Harrington’s study, Scull’s more vivid account demonstrates that the foundations of biological psychiatry were built on violence inflicted on the bodies of women, the poor, and people of color. During the period from 1910 to 1950 in the United States, Scull argues, researchers treated their vulnerable patients “as objects, not sentient beings.” With few legal rights at the time, patients had little recourse for protesting doctors’ invasive and haphazard experiments on their bodies.
Take the American psychiatrist Henry Cotton, who appears in both Harrington and Scull’s accounts. In the 1910s and ’20s, Cotton was convinced that all psychosis was septic in origin—a result of an infection—because it had been demonstrated that one condition, called “general paralysis of the insane,” was caused by the syphilis spirochete Treponema pallidum in the brain. Based on this unproven theory of septic psychosis, Cotton concluded that psychosis could be treated by the surgical removal of potential sources of infection from patients’ bodies. Cotton maimed and killed thousands of patients as he surgically removed teeth, appendices, ovaries, testes, colons and more in the name of curing psychosis. The death rate of Cotton’s colectomies was later determined to be more than 44 percent, with women representing a disproportionate number of his victims.
Another example Scull examines is the Viennese physician Julius Wagner-Jauregg, who thought that inducing high fever and convulsions might help psychiatric patients. He won the Nobel Prize of Medicine in 1927 for using malaria to induce high fever to treat patients with general paralysis of the insane. Harrington points out that at the famous St. Elizabeths Hospital in Washington, D.C., certain patients with chronic psychosis, who were among the most socially marginalized, were turned into “malaria reservoirs” who stored the parasite in their bodies so that it could be distributed to other patients.
Scull suggests that the most extreme experiment during this period was lobotomy. The procedure initially involved applying local anesthesia to the head, drilling through the skull, and cutting the frontal lobes of the brain with a blade. The surgeon stopped cutting the brain when the patient began to get “confused.” The innovation earned Portuguese neurologist Egan Moniz a Nobel Prize of Medicine in 1949. Walter Freeman, who popularized the procedure in the United States, later innovated an approach that required insertion of an ice pick through each eye socket into the brain. Lobotomies were performed by the tens of thousands in the 1940s and ’50s, again disproportionately on women. Freeman described the effects of the procedure as changing his patients into people who were more like “domestic invalid or household pet” so that their behavior was easier for families and institutions to control.
Sterilization was another invasive procedure popularized in American psychiatry during this period. Based on older theories of degeneracy, sterilization was a eugenic rather than therapeutic tool: it was meant to keep people with mental illness from passing on their “bad stock.” The ethically fraught practice made its way to the Supreme Court in the infamous Buck v. Bell case in 1927, when Associate Justice Oliver Wendell Holmes, Jr., argued that society was justified in seeking to “prevent those who are manifestly unfit from continuing their kind.” In the decade that followed the decision, some 28,000 Americans diagnosed with “feeble-mindedness” were sterilized.
Scull and Harrington conclude that the only effective treatment that psychiatry today has inherited from this period of frenzied and dangerous experimentation is electroconvulsive therapy (ECT). Believing (falsely) that seizure disorders and schizophrenia were antagonistic diseases, the Hungarian psychiatrist Ladislav Meduna sought to induce seizures with the powerful stimulant Metrazol in schizophrenic patients in the 1930s. As a result of the sheer violence of the treatment, about 40 percent of patients suffered compression fractures of their spines. The practice was adapted over time to make it safer for patients, eventually evolving into ECT, which continues to be used in American psychiatry today. Current research demonstrates that ECT is safe and effective in the treatment of depression, but like researchers in the 1930s, we still do not know why or how it works.
Rejecting this violent experimentation on the body, the next crop of psychiatric revolutionaries turned, instead, to an approach that focused solely on the mind: psychoanalysis. Sigmund Freud arrived in the United States in 1909, but his ideas did not take hold in the profession until after World War II. Experiences treating traumatized soldiers taught psychiatrists that the war’s psychological wounds could be just as devastating as their physical injuries.
Psychoanalysis developed what Scull calls a “fragile hegemony” over the field in the postwar period. Harrington emphasizes that psychiatrists turned to Freud’s work because they believed it provided a distinctly medical approach to mental illness: an intervention, namely psychoanalysis, elucidated and treated the underlying cause of the patient’s symptoms in the unconscious. By the 1950s most psychiatry residency training programs in the United States were led by psychoanalysts, and many influential analysts consolidated their professional power by denigrating earlier somatic approaches. In 1948, for example, an influential group of analysts argued that lobotomy was not a therapy but rather a “man-made self-destructive procedure that specifically destroys” parts of the brain essential to humanity. Figures in popular culture also saw psychoanalysis as a solution to broader problems facing American society. At the annual conference of the American Psychiatric Association in 1948, President Harry Truman stated that “experts in the field of psychiatry” were essential for safeguarding American “sanity,” which was the “greatest prerequisite for peace.”
But like the boom and bust of revolutions before it, psychoanalysis failed to deliver on its overambition, and the almost exclusive focus on the mind did little to prevent psychiatric harm against vulnerable communities. In the 1970s gay activists vocally protested the pathologization of their sexuality in American psychiatry. These activists, including some gay psychiatrists, stormed the annual conferences of the American Psychiatry Association (APA) and successfully demanded the removal of homosexuality from the profession’s catalogue of disorders.
The problem for activists in gay, feminist, Black Power, and disability movements in the 1970s was that institutional psychoanalysis embraced and conformed individuals to white, ableist, heterosexual, and upper middle-class norms. For those whose identities challenged such norms, psychotherapy was more likely to harm than heal. As members of the Chicago Gay Liberation Front proclaimed in a 1970 leaflet written to the American Medical Association:
We homosexuals of gay liberation believe that the adjustment school of therapy is not a valid approach to society. . . . Mental health for women does not mean therapy for women—it means the elimination of male supremacy. Not therapy for blacks, but an end to racism. The poor don’t need psychiatrists (what a joke at 25 bucks a throw!)—they need democratic distribution of wealth. OFF THE COUCHES, INTO THE STREETS!
Their call to abandon the couch for the street was an indictment of an academic psychoanalytic profession, composed largely of white men, that had reified, instead of challenged, structures of oppression in American society. Many American analysts at mid-century held the belief, for example, that Black people did not possess the psychological sophistication required for psychoanalytic work on the couch. Furthermore, historian Martin Summers has shown that in institutions that treated Black patients, psychoanalysts reinforced older, racist stereotypes of a “distinctive black psyche,” even in the face of data and clinical experience that undermined such a notion.
To be sure, more radical visions of psychoanalysis emerged in the political fervor of 1960s and ’70s, but you have to look beyond Scull and Harrington’s accounts to find them. In the French colony of Algiers, for example, Martinique-Born psychiatrist Frantz Fanon famously critiqued the anti-Black violence of colonialism to imagine more liberatory forms of care. And in Latin America, my own work has shown how Marxist psychoanalysts in the early 1970s imagined a “psychotherapy of the oppressed” that tied mental health to social and political liberation from capitalism and U.S. imperialism. But these radical efforts in the Third World were far removed, geographically and politically, from the mainstream psychoanalysis discussed in these two books.
For Scull and Harrington, perhaps the most damning blow to the legitimacy of American psychiatry came from within the profession itself. In 1973 forensic psychiatrist David Rosenhan published an experiment, titled “On Being Sane in Insane Places,” in the journal Science. His famous study concluded that psychiatrists could not distinguish sanity from insanity. For the experiment, Rosenhan sent eight “pseudo-patients” who pretended to hear the words “empty,” “dull,” and “thud” for interviews at psychiatric hospitals. Rosenhan found that all eight were admitted to the hospital by psychiatrists; their average length of stay was nineteen days. All but one of the patients were given a diagnosis of schizophrenia on discharge. Journalist Susannah Cahalan has more recently shown that Rosenhan fabricated many of his results, but at the time the paper shook the foundations of the profession and broke psychoanalysis’ tenuous grip on the field.
Enter the biological psychiatrists of the 1980s, who laid the groundwork for the biological revolution we find ourselves in today. Partly in response to Rosenhan’s study, this new coalition of psychiatrists blamed the crisis in professional legitimacy on psychoanalysis. Its obscurantist theories, they argued, were more jargon than substance and had turned American psychiatry into a Tower of Babel, where psychiatrists could barely communicate meaningfully with each other. Research from as early as the 1960s showed that diagnosis among psychiatrists was not reliable statistically—that is, psychiatrists often disagreed on diagnosis even when assessing the same patient. The influential psychiatrist Robert Spitzer believed that the solution was to radically reform a book that most professionals had ignored: the DSM. Spitzer and the DSM-III Task Force gutted the psychoanalytic underpinnings of the manual and replaced it with what they believed were clear and objective criteria for each illness based on observable aspects of patient behavior that could guide treatment and research.
The publication of the third edition of the DSM in 1980 heralded the birth of what proponents explicitly called a “biological revolution” in psychiatry. For evidence of this revolution, Spitzer and others pointed to developments in psychopharmacology, especially the introduction of the first effective antipsychotic chlorpromazine in 1954 and biological research that examined the role of neurotransmitters and genetics on mental illness. Research on the brain and the body, they believed, would eventually connect the diseases described behaviorally in the DSM-III to their underlying biological causes.
We now know that this hoped-for science never arrived; psychiatry keeps waiting for its biological Godot. While the DSM-III and subsequent editions, including IV and 5, have improved diagnostic reliability, psychiatry continues to suffer from the problem of validity. In other words, the collection of symptoms that defined each condition in the DSM have still—after billions of dollars of investment—not been correlated with robust changes in our brains, blood, or genes.
The oft-cited claim, for example, that schizophrenia has a genetic basis has failed to pass scientific muster. As Scull discusses, after failing to find a Mendelian set of genes that could explain schizophrenia, researchers in the 2000s pinned their hopes on new genome-wide association studies (GWAS) that could investigate hundreds of thousands of base pairs in the search for genetic linkages to psychiatric disorders. But GWAS studies have not revealed a clear genetic basis for schizophrenia (or bipolar disorder, for that matter). While combining hundreds of genetic sites can help explain, at best, 8 percent of the observed variance of schizophrenia, it is still possible for an individual to have many of these genetic variations without developing the disease. Prominent psychiatrists Michael Rutter and Rudolf Uher have reflected on the disappointment: “Molecular genetic studies of psychiatric disorders have done a lot to find very little. In fact, in the era of genome-wide association studies, psychiatric disorders have distinguished themselves from most types of physical illness by the absence of strong genetic associations.”
While the turn to biology has not meaningfully impacted diagnosis or treatment, it has been wildly successful as a marketing strategy for psychopharmaceuticals. In fact, the most significant change in psychiatry over the last half-century might be the birth of Big Pharma, not any revolution in biology. Psychiatric markets were attractive to pharmaceutical companies for at least two reasons in the 1980s. First, psychotropics are taken over long periods of time: many patients are life-long consumers. Second, self-perception and subjective experience play major roles in the diagnosis of mental illness. This fact, pharma executives realized, means that demand can be influenced and manipulated by effective marketing that positions drugs as a solution to consumers’ dissatisfaction with their lives.
In the 1990s drug companies invested millions to create direct-to-consumer advertisements that capitalized on the biological fervor of academic psychiatrists. These ads claimed, misleadingly, that their drugs targeted “chemical imbalances” in the brain that cause everyday feelings of depression and anxiety in Americans. In addition to consumer demand, the industry also focused their considerable influence on prescribers. Pharma offered influential physicians at prestigious academic centers drug samples, lucrative consulting gigs, and other incentives to peddle their products.
Today the industry financially supports almost every journal and scientific meeting in psychiatry. Some 69 percent of the members of the Task Force of the current DSM-5 disclosed financial ties to the pharmaceutical industry—a 21 percent jump from disclosures reported by the Task Force for DSM-IV. Pharma’s influence on the DSM has contributed to an expansion of diagnostic categories so that the concept of “mental illness” itself has become more inclusive, increasing the size of potential drug markets.
Over the last half century, pharma has also influenced the federal approval of drugs by the Food and Drug Administration (FDA). Today, the FDA gets 46 percent of its budget from companies filing drug applications (so-called “industry user fees”), and companies conduct the safety and efficacy trials on the drugs that they produce. This obvious conflict of interest has led pharma to distort evidence of safety and efficacy, hide negative results and side effect data, and hire ghostwriters to pen academic articles. While a number of major civil and criminal rulings have punished companies for these offenses, the structural source of this unethical behavior—the fact that the industry evaluates the products that it profits from—remains today.
Big Pharma’s heavy influence on the profession has played a major role in shifting the identity of the American psychiatrist—from a psychoanalyst at mid-century to a prescriber of pharmaceuticals today. While research has shown that psychotherapy is just as, or more, effective than drugs for anxiety, depression, and other disorders, psychiatrists generally focus on the prescription of drugs and send patients to psychologists and social workers for therapy. And this shift has paid off handsomely. The psychotropic drug industry today is worth almost $60 billion, and one in six Americans took a psychiatric medication in the last year.
But if the pharmaceutical industry has invested so heavily in psychiatry, why have there been no breakthroughs in drug treatment? A major reason is that the industry has spent billions of dollars more on advertising psychiatric medications than on research and development of novel drugs. As psychiatrist David Healy has shown, money earmarked for R&D is often not intended to produce genuine innovation. Almost all of the psychopharmaceuticals produced since 1990 have been “copycats” that mimic older, generic pharmaceuticals, with only minor chemical modifications. These (unfortunately named) “me-too” drugs work no better clinically than the drugs that came before them, but their slight biochemical novelty means that they can be patented, so that pharma can charge insurance companies’ top dollar.
Perhaps the worst news is that Big Pharma, having created and capitalized on psychiatric markets, is now jumping ship. Anthropologist Joe Dumit has shown that most psychiatric drugs will soon go off patent, so companies will be forced to charge less for them. With the market already saturated with pharmaceutical copycats and no significant scientific biological breakthroughs in sight, there is suddenly little room for growth. Almost all of the major pharmaceutical companies have decided to divest from psychiatric drug research and turn to more promising sectors, especially the development of “biologics” and other cancer drugs.
Does psychiatry, then, have a future? With the pharmaceutical well running dry, Harrington and Scull offer few solutions beyond vague statements about the need for humility in academic psychiatry and the message that psychiatrists should focus on psychosocial, not just biological, approaches to treatment.
Scull also wonders whether a return to psychotherapy might be the answer. Outpatient psychiatry in the United States today is often based on brief, fifteen- to thirty-minute visits that narrowly focus on medication management and symptom check lists. Scull laments the loss of connection that psychoanalysis represented for some (mostly privileged) American patients at mid-century—at least psychiatrists listened to patients in the 1950s, he emphasizes.
Unfortunately, psychotherapy in the last fifty years has become more pill-like itself: standardized, quick, corporate, and cheap. In the 1980s and ’90s, managed care magnified the critiques of some psychiatrists that the intensive and exploratory nature of long-term psychoanalysis was a large investment in time and money with modest gains. They advocated for faster and more affordable forms of care that included not only drugs but also new cognitive-behavioral therapy (CBT) techniques that, as historian Hannah Zeavin has argued, devalued the healing power of the therapist herself. Certain CBT approaches attempted to reduce therapists’ role to largely automated dialogue and manualized programs defined in workbooks and computer programs written for each disorder. In the CBT model, the patient’s thoughts and feelings were understood as scripts that could be reprogrammed, while the introspection and psychological insight—the “listening” valued by Scull—was denigrated by some practitioners as navel-gazing. As a result, traditional psychoanalysis has become almost impossible to come by today. While many therapists adopt an eclectic approach that borrows insights from CBT and various strands of psychoanalysis in practice, the kind of long-term, open-ended therapy that traditional psychoanalysis represented is extremely difficult to access now. Insurance refuses to cover it, and patients who want psychoanalysis are often forced to pay high fees out-of-pocket.
With the decline of psychoanalysis, therapy has continued to verge toward corporate automation. Psychologists and social workers today often search for “gig work” across growing digital platforms like Talkspace to earn around $25 an hour with little control over their hours, fees, or working conditions. Others engage in therapy with an artificially intelligent (and usually feminized) chatbot. Disturbingly, these digital apps are largely unregulated and have questionable standards of care. Given financial pressure from insurance companies and a health system that demands quick fixes, the future of psychotherapy frankly looks bleak—both for patients who desire human contact and for providers whose labor is being devalued to the point of automated erasure.
The only real source of excitement on psychiatry’s horizon seems to be psychedelics, which Harrington mentions very briefly in her conclusion. Non-profit organizations and academic researchers are currently conducting over fifty FDA trials of MDMA (ecstasy), psilocybin (magic mushrooms), LSD (acid), mescaline, ibogaine, and ayahuasca for a wide range of psychiatric disorders. Esketamine has already been approved for treatment-resistant depression. Researchers and journalists, such as Michael Pollan, have dubbed these developments a “psychedelic renaissance” that will revolutionize psychiatry, open new understandings of the connection between mind and brain, and provide benefit to thousands of patients.
But doesn’t this sound all too familiar? The “psychedelic renaissance” feels like the next Harringtonian revolution, with its bombastic claims, massive financial investment, and at this point, uncertain benefit for patients. The verdict is still out about efficacy, but what is already clear is that the pharmaceutical industry has taken notice. In 2020 London-based Compass Pathways, which received seed investment from Peter Thiel’s Thiel Capital, was the first psychedelic pharmaceutical company to go public, with a post-IPO run-up valuation of $1.1 billion.
Not to be left out, Big Pharma is also up to its usual tricks. As I have noted elsewhere, Johnson & Johnson was interested in ketamine’s benefit for depression but could not patent the drug, because it was already a cheap generic. J&J decided to make a copycat, chemically isolating one of the compound’s mirror images. They called this “me-too” compound “Spravato,” patented the drug, and now, charge almost one thousand dollars per dose. Companies are already using similar tactics to isolate patentable compounds from psychoactive botanicals that Indigenous communities have used for centuries, raising ethical concerns about how the burgeoning psychedelic industry perpetuates Euro-American exploitation of Indigenous knowledge, plants, and land in settler colonies.
This “psychedelic renaissance,” then, is likely just the next stage of the larger revolution in Big Pharma that started in the 1980s. And whatever clinical benefit psychedelics end up offering, drugs are not a solution for the structural problems that plague our mental health system. Big Pharma, and the academic psychiatrists who partner with industry, will continue to profit. And psychedelics can only help those who have access to them in our society: mostly white, upper middle-class people with private insurance.
While both of these impressive books cover significant historical ground, they also miss something critical about psychiatry’s past that limits their vision of its future: they fail to confront the profession’s role in the mass incarceration of the Black community over the last half-century. For Harrington and Scull, carceral approaches to psychiatry largely came to an end, at a population level, with the closure of large asylums and the rise of deinstitutionalization—a movement in the 1960s that attempted to transition care from psychiatric hospitals to communities. In this common narrative, the problem with deinstitutionalization was one of neoliberal neglect: patients were discharged en masse from institutions with few resources and little support, leading to high rates of homelessness among people with serious mental illness.
But this story overlooks the silent and subtle ways that incarceration has become further intertwined with psychiatry. As historian Anne Parsons has argued, “the asylum did not disappear” with deinstitutionalization. Instead “it returned in the form of the modern prison industrial complex.” Some of the largest mental health centers in the country currently operate in prisons, and today, there are more people with serious psychiatric illness in America’s prisons than in its remaining psychiatric hospitals. Around 40 percent of people diagnosed with serious mental illness will face incarceration in their lifetimes, in many cases, as a consequence of the racist policies that undergird the ongoing War on Drugs. This carceral mental health is highly segregated. While psychiatric hospitals tend to house white, middle-aged patients, prisons disproportionately confine people with psychiatric disorders who are Black and under the age of forty.
Moreover, sociologist Anthony Ryan Hatch has argued that the use of prison psychopharmaceuticals has allowed for incarceration at the level of the brain. Prison-policy strategists have framed psychopharmaceuticals not as medical treatments but rather, as an important component of technocorrections, that is, “the strategic application of new technologies in the effort to reduce the costs of mass incarceration and minimize the risks prisoners pose to society.” In 2000, some 95 percent of maximum or high-security state prisons were distributing psychiatric drugs to incarcerated people.
These facts are missing from these books because both Harrington and Scull are ultimately focused on elite academic psychiatrists—a community that tends to avoid work in prisons. As Hatch notes, almost all of our public knowledge about psychopharmaceuticals comes from their use among the unincarcerated, while knowledge about prison psychotropics tends to be as tightly guarded as inmates themselves. This silence is a form of oppression that covers up both the use of psychotropics as a technology of custodial control and the failure to provide people in prison—many of whom are traumatized by their incarceration—with the humane treatment that they deserve.
As a psychiatrist myself, I believe that an important part of this tragedy is the silence and lack of accountability among those who represent our field. Despite the decreasing life expectancy of people with mental illness, high rates of incarceration and homelessness, and the failure of the biological paradigm, the biopsychiatric research machine just keeps growing. In his own new book, Healing: Our Path from Mental Illness to Mental Health, Insel argues that the failures of biological psychiatry’s past indicate that we should “double down on brain research” instead of re-examining our priorities. Insel’s successor at the NIMH, Joshua Gordon, has maintained the organization’s focus on biopsychiatric research, narrowly construed. While both Harrington and Scull point to a “crisis” in the profession today, the scarier truth is that many in the academy are proceeding with business as usual. The real crisis in academic psychiatry, in other words, is that there is no crisis.
If these histories of elite academic practitioners do not show us the whole problem, they are also not going to produce imaginative solutions. Searching for answers requires de-centering the academy and looking to narratives that have largely been neglected in standard histories of psychiatry. The historical work of disability activist and scholar Liat Ben-Moshe, for example, turns to Mad communities who have embraced neurodivergence not as a medical problem that needs to be fixed but as an identity that should be celebrated. Mad activists and professional allies in the 1970s, such as the antipsychiatrist Thomas Szasz, successfully demanded the abolition of violent psychiatric hospitals and carceral practices in American society. While this movement to deinstitutionalize psychiatry did not result in wholesale liberation of people with disabilities in the United States, Ben-Moshe argues that it offers important lessons about how communities can successfully resist the structures that repress them in the name of care.
Ben-Moshe’s work not only provides a means for critically examining the psychiatric violence of the past but also offers what she calls “genealogies” for thinking about futures that seem otherwise unimaginable. Genealogies of resistance conceptualize “health” not in terms of access to individualized treatment provided by academic physicians but rather in terms of collective liberation from the structural conditions that produce the vast extent of psychological suffering and trauma. These genealogies undergird the work of communities and professionals fighting today to abolish the carceral system and to imagine non-violent forms of care through peer support, soteria houses, and political protest. In Los Angeles last year, for example, a vocal coalition of community organizers, academics, and officials successfully stopped the construction of a “psychiatric jail” and advocated for the reinvestment of those funds into initiatives for community-based mental health care. “Care first, jails last,” they are demanding.
There are also unexpected lessons here for more privileged communities. Material wealth does not completely insulate people from the psychological damage of capitalism, of course. Burnout and depression are endemic among upper middle-class physicians and medical students, to name only one example. Over a third of students at Yale, many of whom come from privileged backgrounds, seek mental health services for psychic distress. As psychotherapist Gary Greenberg has bluntly put it, “The fact is, if we didn’t have such a fucked-up society, I’d be out of a job.” Psychological suffering in the upper crust of society is not only evidence that we need increased access to care, whether through pharmaceuticals or psychotherapy. It is also a call to mobilize against the pathogenic features of our local social climates, from toxic training programs and high-pressure university cultures to dehumanizing factory floors. As historian Joanna Radin encouraged me to discuss in my undergraduate course on the History of Drugs, the question is not only, What is the right drug for me?, but also: What would the world have to look like for me not to need drugs at all?
Harrington and Scull surely did not intend for their books to be read this way, but we might understand them as a call to defund biological psychiatry in the United States—to refuse yet another promise of a “revolution” or “renaissance” that would save an academic project that has done little to help and lots to harm. We do not need to be neuroscientists to know that psychological and emotional suffering is “real” or “legitimate,” and that a pill, however effective, cannot abolish the carceral and capitalist system that is the source of so much trauma. As these books teach us, psychiatric paradigms are fragile, and perhaps biology’s tenuous grip on the profession is finally easing under the strain of recent critiques. The future of our profession, if it has one, does not lie in tired promises of biological breakthroughs. It depends on unearthing and embracing neglected histories and genealogies of solidarity with the communities that academic psychiatry claims to serve.